Dr Melanie Rees-Roberts

DE-eSCALation of opioids post-surgical dischargE - The role of clinical pharmacists in reducing opioid dependence at the interface between hospital and primary care
Opioids are very strong painkillers that are often given to treat severe short-term pain, such as after having surgery. These drugs are very good at short-term pain relief. However, used longer than the recommended 2–4 weeks, they can cause more pain, become addictive and/or lead to death.
Studies in the USA found that taking opioids for longer than a week doubles a person’s risk of using them for more than a year, doubling again if used for over a month. Furthermore, patients receiving high-strength opioids following minor or major surgery were more likely to use them long-term, even if they had never taken this type of medicine before.
Not much is known about opioid prescribing in UK hospitals following surgery and the link with harmful long-term use. Records show that in 2017-2018, 5.6 million opioid prescriptions were dispensed in the UK, equivalent to approximately 13% of the adult population. Given the risk of long-term use of opioids post-surgery and with over 4.7 million UK surgical procedures occurring every year, more knowledge of practices and support needed for surgical patients is needed.
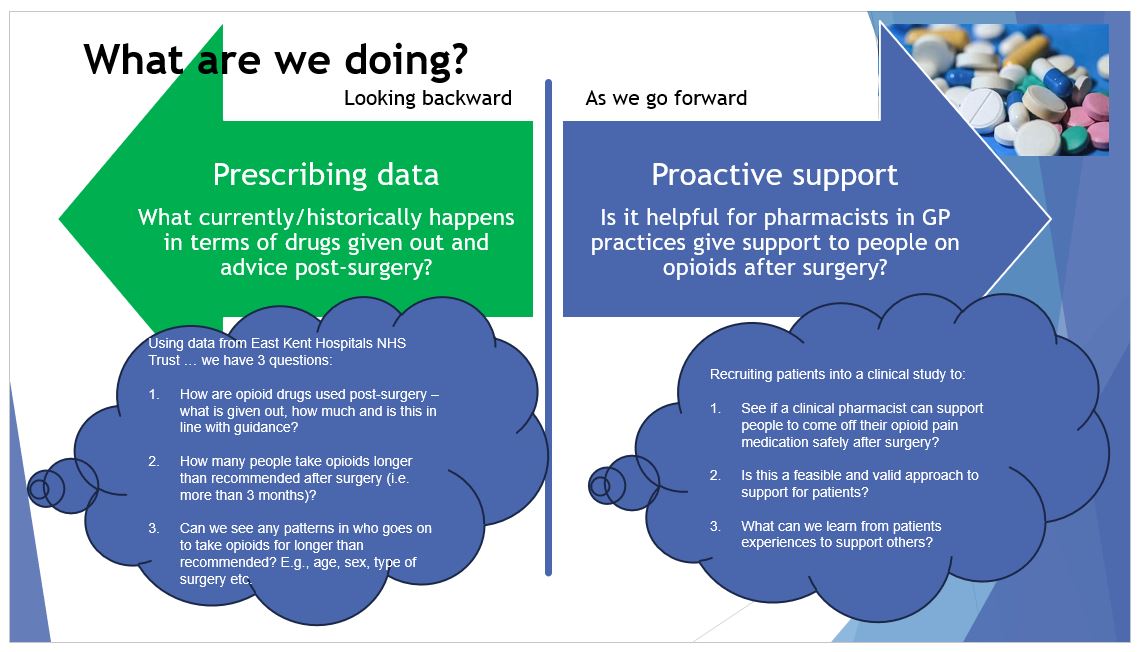
This research project will look at the prescribing trends of opioids and if this is linked significantly to long-term use following surgery within East Kent. The project has two components:
- A retrospective study using pseudo-anonymised routinely collected healthcare data to understand opioid prescribing after surgery and its link to longer use.
- A prospective clinical study to see if it is feasible and acceptable to support patients to come off their opioid medication post-surgery by talking to and getting support from a clinical pharmacist in their GP practice.
The project is working closely with key stakeholders, such as patients, clinical pharmacists and senior healthcare professionals to support the running of the project, such as for recruitment, data collection and sharing findings but also help us better understand how the intervention might work over the longer term.
To reach a wider audience the results will be written for NHS websites/newsletters, community magazines, and academic journals.
If you are interested in taking part in the research, you can read our participant information sheet here: Participant Information Leaflet Supporting Safe Use of Opioid Medication after Surgery
Public Involvement partners/group input
Three NIHR Research Champions from KCHFT provided thoughts and insights into the research idea, design and project overall.
Two public contributors will be part of the research team (including a patient with experience of long-term opioid use), joining monthly project meetings and embedding their support and work throughout. The PPIE lead will maintain regular and accessible communication, identify, and address any training needs, and along with the research team, work together with the public contributors.
Examples of activities include reviewing ethics and governance documents, advice and insights into recruitment and delivery of the research activities, preparing lay summaries of the findings, and dissemination activities. Depending on personal preference they could also get involved in patient interviews and data analysis. PPIE activities will be logged to capture all aspects of involvement and demonstrate impact.
We will invite a wider stakeholder group of patients, clinical pharmacists, primary (GPs) and secondary healthcare professionals to share their thoughts of the deprescribing intervention and, if successful, how it could be implemented in the longer term and successfully scaled up.
Funding: NIHR ARC KSS – priorities for care call
Who is involved
- Dr Emma Veale, Medway School of Pharmacy, Principal Investigator
- Dr Johanna Theron, Kent Community Health Foundation Trust, Principal Investigator
- Dr Melanie Rees-Roberts, CHSS, Co-Investigator
- Ellie Santer, CHSS, Co-Investigator
- Dr Julie Hedayioglu, Kent Community Health Foundation Trust, Co-Investigator
- Start date 1/4/2022 End date 30/9/2024